
Cancer diagnosis and staging are crucial steps in understanding the extent of the disease and planning the most effective treatment. Early and accurate diagnosis can significantly improve treatment outcomes, while staging helps determine how far the cancer has spread. A thorough history-taking and clinical examination form the foundation of cancer diagnosis. This step involves: A biopsy is the gold standard for confirming cancer. This involves extracting a tissue sample from the suspected tumor site and examining it under a microscope. Common biopsy techniques include: Tumor markers are substances produced by cancer cells or by the body in response to cancer. These markers help in diagnosis, prognosis, and monitoring treatment response. Some commonly used tumor markers include: Molecular and genetic testing help identify specific mutations that drive cancer growth. This information is vital for selecting targeted therapies that inhibit cancer-promoting pathways. Examples include: Staging determines how much cancer has spread and helps choose the appropriate treatment plan. The key imaging modalities used in staging include: Cancer staging plays a critical role in determining treatment options. It helps oncologists decide whether a patient needs surgery, chemotherapy, radiation, or a combination of therapies. Accurate cancer diagnosis and staging are essential for developing an effective treatment plan. With advancements in biopsy techniques, tumor markers, molecular testing, and imaging technologies, oncologists can make informed decisions to improve patient outcomes. Early detection, personalized therapy, and continuous monitoring through innovative diagnostic tools offer hope for better cancer management and survival rates.1. Detailed History-Taking and Clinical Examination
,
,2. Ordering and Interpreting Biopsy & Histopathology Reports
,
,3. Tumor Marker Analysis and Liquid Biopsies
,
,4. Molecular & Genetic Testing for Targeted Therapy Selection
,
,5. PET-CT, MRI, and Other Imaging Studies for Staging
,
,The Importance of Staging in Cancer Treatment
,
,Conclusion
,
Cancer treatment has evolved significantly over the years, with systemic anti-cancer therapy playing a crucial role in managing and treating various types of cancer. Systemic therapy involves the use of medications that travel through the bloodstream to reach and affect cancer cells throughout the body. This article explores different types of systemic anti-cancer therapies, including chemotherapy, targeted therapy, immunotherapy, hormonal therapy, and combination therapy. Chemotherapy is one of the most well-known and widely used systemic anti-cancer treatments. It involves the use of powerful drugs to kill or slow down the growth of cancer cells. Chemotherapy can be classified into three main types based on its purpose: Administered before the main treatment, such as surgery or radiation therapy, to shrink tumors and make them easier to remove. Commonly used in breast cancer, lung cancer, and sarcomas. Given after primary treatment to destroy any remaining cancer cells and reduce the risk of recurrence. Often used in breast, colon, and ovarian cancers. Used in advanced or metastatic cancers to relieve symptoms, slow disease progression, and improve quality of life. Targeted therapy is a revolutionary approach that specifically attacks cancer cells while minimizing damage to normal cells. It works by targeting molecular changes that drive cancer growth. These drugs interfere with specific proteins and pathways that promote cancer cell survival and proliferation. Examples include tyrosine kinase inhibitors (TKIs) like imatinib and EGFR inhibitors like erlotinib. These are lab-made molecules that bind to specific cancer cell markers, blocking their growth or triggering the immune system to attack them. Examples include trastuzumab (for HER2-positive breast cancer) and rituximab (for lymphoma). Immunotherapy enhances the body’s immune system to recognize and attack cancer cells. It has shown remarkable success in treating various cancers. These drugs block proteins like PD-1, PD-L1, and CTLA-4, which help cancer cells evade immune detection. Examples include pembrolizumab and nivolumab. This therapy involves modifying a patient’s T cells to better recognize and attack cancer cells. It has been a breakthrough treatment for leukemia and lymphoma. Hormonal therapy is specifically used to treat hormone-sensitive cancers by blocking or lowering hormone levels that fuel cancer growth. For hormone receptor-positive breast cancer, drugs like tamoxifen and aromatase inhibitors help reduce estrogen levels and slow cancer progression. Prostate cancer growth is often driven by androgens. Androgen deprivation therapy (ADT) using drugs like leuprolide lowers testosterone levels to control cancer growth. Combination therapy involves using two or more treatment modalities to enhance effectiveness. The combinations are designed to maximize cancer cell destruction while minimizing resistance and side effects. Combining chemotherapy with immunotherapy has shown promising results in treating lung cancer, Hodgkin’s lymphoma, and other cancers. Combining different targeted therapies can block multiple pathways simultaneously, making it harder for cancer to develop resistance. Some cancers respond well to a combination of chemotherapy and targeted therapy. Systemic anti-cancer therapy has revolutionized the way we treat cancer, offering more effective and personalized treatment options. Advances in chemotherapy, targeted therapy, immunotherapy, hormonal therapy, and combination therapies have significantly improved survival rates and quality of life for cancer patients.1. Chemotherapy
,2. Neoadjuvant Chemotherapy
,3. Adjuvant Chemotherapy
,4. Palliative Chemotherapy
,5. Targeted Therapy
,6. Small Molecule Inhibitors
,7. Monoclonal Antibodies
,8. Immunotherapy
,9. Checkpoint Inhibitors
,10. CAR-T Cell Therapy
,11. Hormonal Therapy
,12. Breast Cancer Hormonal Therapy
,13. Prostate Cancer Hormonal Therapy
,14. Combination Therapy
,15. Chemo-Immunotherapy
,16. Targeted Therapy Combinations
,17. Chemo-Targeted Therapy
,Conclusion
,
In the ever-evolving landscape of healthcare, Personalized & Precision Medicine (PPM) is revolutionizing cancer treatment by tailoring therapies to individual patients. Unlike traditional approaches that apply generalized treatments, PPM integrates biomarker identification, genomic profiling, and AI-driven predictive models to design highly effective therapeutic strategies. This approach enhances treatment efficacy, minimizes adverse effects, and improves patient outcomes. Biomarkers are measurable indicators of biological processes, disease states, or responses to therapy. In oncology, they play a crucial role in diagnosing cancer, predicting prognosis, and guiding treatment decisions. The identification of specific biomarkers enables oncologists to customize treatments that align with a patient’s unique genetic makeup. Genomic profiling is a powerful tool that analyzes a patient’s tumor DNA to identify mutations driving cancer growth. This allows oncologists to tailor treatments based on genetic alterations rather than a one-size-fits-all approach. Artificial Intelligence (AI) is transforming oncology by analyzing complex datasets to predict the best treatment options for patients. Personalized & Precision Medicine is revolutionizing cancer care by leveraging biomarkers, genomic profiling, and AI-driven predictive models. These advancements are enabling oncologists to design tailored treatments that maximize efficacy while minimizing side effects.Understanding Biomarkers in Cancer Treatment
, Key Biomarkers in Cancer Treatment
,,
,Genomic Profiling: Customizing Treatment at the Molecular Level
,Techniques Used in Genomic Profiling
,,
, AI-Based Predictive Models in Therapy Selection
,Benefits of AI in Precision Medicine
,,
,Conclusion
,
Prognostication and risk assessment are critical aspects of oncology, helping medical professionals determine the aggressiveness of a disease, estimate recurrence risks, predict treatment responses, and make informed decisions regarding patient care. With advancements in medical research and technology, modern tools such as nomograms and scoring systems have revolutionized how oncologists evaluate cancer progression and survival rates. Prognostication involves predicting the likely course and outcome of a disease based on various clinical, pathological, and molecular factors. Risk assessment, on the other hand, helps stratify patients based on their likelihood of disease progression or recurrence. These evaluations are essential for devising personalized treatment strategies, optimizing resource utilization, and improving patient outcomes. With advancements in precision medicine, AI, and genomic research, prognostication is becoming more accurate. Liquid biopsies, ctDNA analysis, and AI-driven diagnostics are shaping the future of cancer care. Prognostication and risk assessment play a crucial role in modern oncology. The integration of nomograms, scoring systems, and AI-based models continues to enhance prognostic evaluations, ultimately leading to better patient outcomes and more effective cancer treatments.Understanding Prognostication & Risk Assessment
, Assessing Disease Aggressiveness & Recurrence Risk
,,
, Predicting Treatment Responses and Survival Rates
,,
,Use of Nomograms and Scoring Systems for Decision-Making
,,
,The Future of Prognostication in Oncology
,Conclusion
,

Supportive and palliative care is an essential aspect of modern medicine, focusing on improving the quality of life for individuals facing serious illnesses. It aims to provide relief from pain, manage symptoms, and offer emotional, psychological, and nutritional support. Unlike curative treatments, palliative care prioritizes comfort, dignity, and holistic well-being for patients and their families. Pain is one of the most common and distressing symptoms in patients with advanced illnesses. Effective pain management is crucial to ensuring a patient’s comfort and overall well-being. Several approaches are used to control pain, including: Cancer treatments, such as chemotherapy and radiation therapy, often cause severe side effects that can affect a patient’s quality of life. Palliative care includes strategies to manage these side effects effectively. Nutrition plays a vital role in maintaining strength and immune function in patients with chronic illnesses. Many patients experience loss of appetite due to their medical condition or treatment, leading to malnutrition and weight loss. A serious illness affects not just the physical health of a patient but also their mental and emotional well-being. Addressing psychological and emotional concerns is a crucial aspect of palliative care. Supportive and palliative care is an indispensable part of medical treatment, focusing on providing comfort, dignity, and holistic care to patients and their families. By addressing pain, managing side effects, offering nutritional support, and providing psychological care, palliative care ensures that patients experience the best possible quality of life, even in the face of serious illness. As medical advancements continue, integrating palliative care into standard treatment plans will remain crucial in offering compassionate and comprehensive healthcare.Pain Management in Palliative Care
,,
, Managing Treatment Side Effects
,,
, Nutritional Support and Appetite Stimulants
,,
,Psychological Support and Counseling
,,
,Conclusion
,
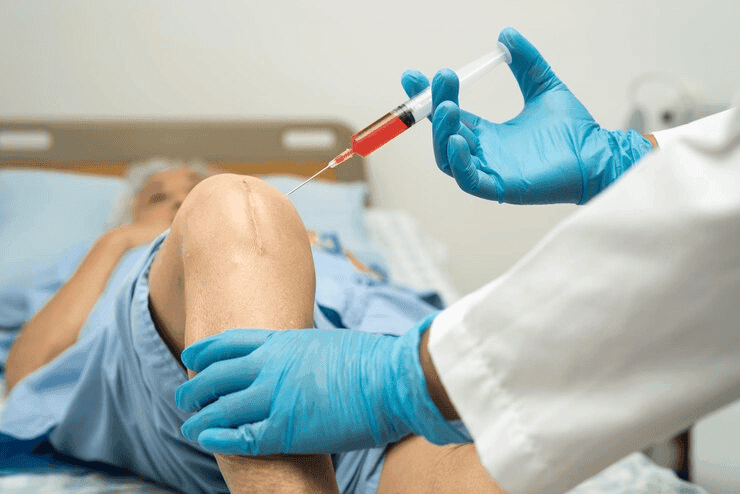
Bone Marrow Transplantation (BMT) and Cellular Therapy have revolutionized the treatment of various hematological disorders and malignancies. These advanced medical procedures have given new hope to patients suffering from leukemia, lymphoma, aplastic anemia, and other life-threatening conditions. BMT involves the replacement of diseased or damaged bone marrow with healthy stem cells, which help restore normal blood cell production. Cellular therapy, including CAR-T cell therapy, offers targeted treatment for certain cancers, significantly improving survival rates and quality of life. In an autologous transplant, the patient’s own stem cells are collected before undergoing high-dose chemotherapy or radiation therapy. These stem cells are then reinfused to restore bone marrow function. This method is commonly used for conditions such as multiple myeloma and certain lymphomas. The advantage of autologous transplantation is the lower risk of immune rejection since the patient’s own cells are used. Allogeneic transplants involve using stem cells from a compatible donor, which could be a sibling, parent, or an unrelated donor. This method is commonly used for treating leukemia, aplastic anemia, and genetic disorders. The success of an allogeneic transplant depends on the compatibility between the donor and recipient, often determined by human leukocyte antigen (HLA) matching. This type of transplant provides a graft-versus-tumor effect, where the donor cells help eliminate any remaining cancer cells in the patient’s body. After an allogeneic transplant, the recipient's immune system needs time to adapt to the donor cells. Immunosuppressive medications are used to prevent graft-versus-host disease (GVHD), a condition where the donor immune cells attack the recipient’s tissues. Post-transplant care includes: Chimeric Antigen Receptor T-cell (CAR-T) therapy is an innovative cellular therapy that has transformed the treatment landscape for blood cancers. It involves genetically modifying a patient’s T cells to recognize and attack cancer cells more effectively. This therapy has shown remarkable success in treating relapsed or refractory leukemia and lymphoma. Patients diagnosed with the following conditions may be eligible for these advanced treatments: Ongoing research in stem cell transplantation and cellular therapy aims to enhance the effectiveness of treatments while reducing complications. Innovations such as gene editing (CRISPR), improved donor matching techniques, and expanded CAR-T cell applications are expected to further improve patient outcomes. The integration of artificial intelligence in predicting transplant success rates and personalized treatment plans is also a promising development in this field. Bone Marrow Transplantation and Cellular Therapy offer a lifeline to patients with severe hematological conditions. Advances in these treatments have significantly improved survival rates and quality of life. As research continues to evolve, the future of regenerative medicine and cancer treatment looks brighter, paving the way for more accessible and effective therapies.Types of Bone Marrow Transplantation
,1. Autologous Stem Cell Transplant
,2. Allogeneic Stem Cell Transplant
, Post-Transplant Immunosuppressive Management
,,
,CAR-T Cell Therapy: A Breakthrough in Hematological Malignancies
,How CAR-T Cell Therapy Works
,,
,Who Can Benefit from BMT and Cellular Therapy?
,,
,Future of Bone Marrow Transplantation & Cellular Therapy
,Conclusion
,

Cancer patients, particularly those undergoing chemotherapy or suffering from advanced malignancies, are susceptible to life-threatening complications known as oncologic emergencies. Prompt recognition and management of these conditions are essential to improve patient outcomes. Below, we discuss some of the most critical oncologic emergencies, their causes, symptoms, and treatment approaches. Febrile neutropenia (FN) is a serious complication that arises when cancer patients, especially those receiving chemotherapy, develop an abnormally low neutrophil count, making them highly vulnerable to infections. Hypercalcemia occurs when calcium levels in the blood become dangerously high, often due to certain cancers such as lung, breast, and multiple myeloma. Spinal cord compression is a devastating complication of metastatic cancer, particularly from lung, breast, and prostate malignancies, which can lead to permanent neurological damage if not treated promptly. TLS is a metabolic emergency caused by the rapid destruction of tumor cells, leading to the release of intracellular contents into the bloodstream, resulting in electrolyte imbalances. SVC syndrome occurs when a tumor obstructs the superior vena cava, leading to impaired venous return from the upper body to the heart. Oncologic emergencies require immediate recognition and swift intervention to prevent life-threatening complications. Healthcare providers should maintain a high index of suspicion in at-risk cancer patients and implement appropriate treatment strategies promptly. Multidisciplinary collaboration among oncologists, emergency physicians, and palliative care teams plays a vital role in optimizing patient outcomes and improving quality of life.1. Febrile Neutropenia and Sepsis
,
,Symptoms:,
,Management:,
,2. Hypercalcemia of Malignancy
,
,Symptoms:,
,Management:,
,3. Spinal Cord Compression
,
,Symptoms:,
,Management:,
,4. Tumor Lysis Syndrome (TLS)
,
,Symptoms:,
,Management:,
,5. Superior Vena Cava (SVC) Syndrome
,
,Symptoms:,
,Management:,
,Conclusion
,
Cancer treatment has evolved significantly over the years, and one of the most impactful advancements in modern oncology is the concept of a Multidisciplinary Tumor Board (MTB). These boards bring together specialists from different fields, ensuring a collaborative approach to cancer diagnosis, treatment planning, and patient care. By fostering open communication between medical professionals, MTBs enhance decision-making processes, leading to improved patient outcomes. A Multidisciplinary Tumor Board is a panel of healthcare professionals specializing in various aspects of cancer care. The primary objective of the board is to review and discuss complex cancer cases and develop comprehensive treatment plans tailored to individual patients. By integrating expertise from multiple specialties, the board ensures that every patient receives a holistic and personalized treatment approach. One of the most crucial aspects of an MTB is the collaboration between surgical and radiation oncologists. These two specialties often work together to determine the most effective course of action for cancer patients. Accurate diagnosis and personalized treatment planning require close collaboration between radiologists, pathologists, and geneticists. Another significant function of MTBs is their role in identifying potential clinical trials and novel treatment options for patients. Cancer research is continuously evolving, and new therapies are being tested to improve survival rates and reduce side effects. The collaborative approach of MTBs provides several benefits for both patients and healthcare providers: While MTBs provide significant advantages, they also present certain challenges: To overcome these challenges, many institutions are adopting virtual tumor boards, allowing specialists from different locations to collaborate remotely. Additionally, AI-driven analytics are being integrated into MTBs to assist in data interpretation and treatment recommendations. Multidisciplinary Tumor Boards represent a cornerstone of modern oncology, ensuring that cancer patients receive the best possible care through expert collaboration. By uniting surgical and radiation oncologists, radiologists, pathologists, geneticists, and other specialists, these boards facilitate informed decision-making, enhance treatment precision, and improve patient outcomes.The Role of a Multidisciplinary Tumor Board
,Key Participants in an MTB
,,
,Collaboration Between Surgical and Radiation Oncologists
,Surgical Oncology Contributions
,,
,Radiation Oncology Contributions
,,
,Joint Decision-Making with Radiologists, Pathologists, and Geneticists
,Discussion of Clinical Trials and Novel Treatment Options
,Benefits of Multidisciplinary Tumor Board Participation
,For Patients:
,,
,For Healthcare Providers:
,,
,Challenges and Future Directions
,,
,Conclusion
,

Cancer remains one of the most challenging diseases in modern medicine, requiring continuous research and innovation to improve treatment outcomes. Clinical trials and research play a critical role in the development of new drugs, biomarkers, and treatment regimens, ensuring that cancer therapies are safe, effective, and tailored to individual patients. This article explores the importance of clinical trials, the process of designing and conducting Phase I–IV trials, and the role of translational research in bringing novel cancer therapies from the laboratory to the clinic. Clinical trials are research studies that evaluate new medical treatments, drugs, or procedures in human participants. They help determine the safety, effectiveness, and potential side effects of new therapies before they become widely available. These trials follow strict guidelines set by regulatory authorities such as the U.S. Food and Drug Administration (FDA) and the European Medicines Agency (EMA) to ensure ethical and scientific integrity. Advancements in cancer treatment rely on the discovery and validation of new drugs, biomarkers, and treatment approaches. Research in these areas helps develop personalized treatment plans tailored to a patient’s genetic and molecular profile. New drug development is a rigorous process that starts in the laboratory and progresses through preclinical studies before entering clinical trials. Promising targeted therapies, immunotherapies, and chemotherapy drugs undergo extensive testing to evaluate their effectiveness in specific types of cancer. Biomarkers are biological molecules found in blood, tissue, or body fluids that indicate the presence of cancer or predict how a patient will respond to treatment. Traditional cancer treatments like surgery, chemotherapy, and radiation therapy are being combined with newer approaches to create more effective regimens. Translational research is a critical field that transforms scientific discoveries into real-world medical applications. It connects basic laboratory research with clinical practice, ensuring that innovative therapies reach patients as quickly as possible. Clinical trials and research have revolutionized cancer treatment, leading to significant breakthroughs in recent years. Some of the key benefits include: Clinical trials and research are the backbone of progress in cancer treatment. From designing and conducting Phase I–IV trials to investigating novel drugs, biomarkers, and treatment regimens, scientists are continuously working to develop safer, more effective therapies. Translational research plays a crucial role in ensuring that these discoveries move from the laboratory to the clinic, offering hope to millions of cancer patients worldwide.Understanding Clinical Trials
,Phases of Clinical Trials
,,
,Investigating Novel Drugs, Biomarkers, and Treatment Regimens
,Development of New Cancer Drugs
,,
,The Role of Biomarkers in Cancer Treatment
,,
,Innovative Treatment Regimens
,,
,The Role of Translational Research
,Key Areas of Translational Cancer Research
,,
,The Importance of Clinical Research in Cancer Treatment
,,
,Conclusion
,

Cancer survivorship begins at the moment of diagnosis and continues through the rest of a patient’s life. The journey from diagnosis to recovery is challenging, but survivorship care ensures that individuals maintain a high quality of life after treatment. Long-term follow-up is essential to monitor late side effects, prevent secondary malignancies, and provide support for lifestyle modifications, psychosocial well-being, and fertility concerns. Cancer treatments such as chemotherapy, radiation, and surgery can have long-term consequences on a survivor’s health. Late side effects may appear months or even years after treatment, making regular monitoring crucial. A healthy lifestyle plays a crucial role in reducing the risk of recurrence, managing long-term side effects, and improving overall well-being. The emotional, social, and reproductive health of cancer survivors is as important as their physical well-being. By adopting a proactive approach to health, cancer survivors can not only manage potential risks but also thrive in their post-treatment life.Monitoring for Late Side Effects & Secondary Malignancies
,,
,Guiding Patients on Lifestyle Modifications
,,
,Psychosocial and Fertility Counseling Post-Treatment
,,
,
Cancer remains one of the leading causes of mortality worldwide, but with advancements in medical research, it is now possible to reduce cancer risks significantly through preventive oncology and screening programs. Preventive oncology focuses on identifying risk factors, implementing early detection strategies, and reducing cancer incidence through lifestyle changes, medical interventions, and awareness programs. This article explores key aspects of preventive oncology, including cancer risk assessment, genetic counseling, high-risk population screening, and chemoprevention. Preventive oncology is a specialized branch of medicine dedicated to reducing cancer risk and preventing cancer development. It involves a multidisciplinary approach that includes lifestyle modifications, medical interventions, and early detection through regular screenings. The goal is to detect cancer at its earliest stages or prevent it from occurring altogether. Cancer risk assessment involves evaluating an individual's likelihood of developing cancer based on personal and family medical history, lifestyle factors, and genetic predispositions. Genetic counseling plays a crucial role in identifying hereditary cancer syndromes and guiding individuals on preventive measures. Cancer screening programs aim to detect cancer at an early, more treatable stage. High-risk populations—individuals with genetic predisposition, family history, or exposure to carcinogens—benefit the most from regular screenings. Mammography is a widely used screening tool for early detection of breast cancer. Women, especially those with a family history of breast cancer or carrying BRCA mutations, are advised to undergo regular mammograms. Early detection through mammography significantly increases survival rates and allows for less aggressive treatment options. Human Papillomavirus (HPV) screening and Pap smears are essential for detecting precancerous changes in cervical cells. Regular screening helps in early intervention, reducing the risk of cervical cancer. A colonoscopy is an effective screening method for detecting colorectal cancer in its early stages. Individuals over 50, or those with a family history of colorectal cancer, are advised to undergo regular screenings. Chemoprevention involves using pharmaceutical agents to prevent or delay cancer development in high-risk individuals. Tamoxifen is a selective estrogen receptor modulator (SERM) that reduces the risk of breast cancer in women with a high genetic predisposition. Preventive oncology and screening programs are crucial in reducing cancer incidence and mortality. Through cancer risk assessment, genetic counseling, regular screenings, and chemoprevention, individuals can take proactive steps to safeguard their health. By embracing preventive oncology, we can move toward a future with lower cancer rates and improved overall well-being.Understanding Preventive Oncology
,Cancer Risk Assessment and Genetic Counseling
,Importance of Genetic Counseling
,,
,Screening Programs for High-Risk Populations
,Mammography for Breast Cancer
,HPV Screening and Pap Smear for Cervical Cancer
,Colonoscopy for Colorectal Cancer
,Chemoprevention: Reducing Cancer Risk Through Medication
,Tamoxifen for Breast Cancer Prevention
,Conclusion
,
Cancer treatment has undergone a paradigm shift in recent years, with technological advancements playing a significant role in improving patient outcomes. The integration of Artificial Intelligence (AI) in digital oncology is revolutionizing how cancer is diagnosed, treated, and monitored. From AI-based treatment algorithms to digital pathology and tele-oncology, these innovations are shaping the future of cancer care. AI-powered treatment algorithms are transforming oncology by enhancing decision-making processes and providing personalized treatment plans. These algorithms analyze vast amounts of patient data, including genetic information, tumor characteristics, and medical history, to predict the most effective treatment strategies. AI-driven platforms assess individual patient profiles and recommend targeted therapies based on predictive modeling. These algorithms help oncologists select the best course of action, reducing trial-and-error approaches and improving treatment efficacy. AI assists in categorizing patients based on their risk levels. By analyzing biomarkers, imaging data, and genetic mutations, AI identifies patients at higher risk for disease progression or recurrence. This enables early interventions and tailored surveillance plans to enhance patient survival rates. AI is accelerating drug discovery by analyzing molecular structures and predicting potential drug candidates. Machine learning models simulate how different drugs interact with cancer cells, expediting clinical trials and bringing new therapies to market faster. Telemedicine is bridging the gap between patients and healthcare providers, particularly in oncology. Tele-oncology leverages digital platforms to provide remote consultations, continuous monitoring, and real-time support for cancer patients, ensuring timely and efficient care. Tele-oncology enables oncologists to consult with patients remotely, reducing the need for frequent hospital visits. This is particularly beneficial for immunocompromised cancer patients who need to minimize exposure to infections. AI-powered remote monitoring tools track patient symptoms, medication adherence, and side effects in real time. Wearable devices and mobile applications collect patient data, allowing oncologists to intervene early in case of complications. Patients in rural or underserved areas often lack access to specialized oncology services. Tele-oncology bridges this gap by connecting patients with leading oncologists, enabling them to receive expert opinions and treatment recommendations without geographic limitations. Advancements in digital pathology and AI-assisted radiology are significantly improving the accuracy and speed of cancer diagnosis. AI-driven tools are assisting pathologists and radiologists in analyzing medical images with greater precision. Digital pathology leverages AI to analyze histopathological slides and detect cancerous cells. AI algorithms identify patterns and anomalies that may be missed by human eyes, improving diagnostic accuracy and enabling early detection. AI-driven radiology interpretation enhances the detection of tumors in imaging scans such as X-rays, CT scans, and MRIs. Machine learning models detect abnormalities, classify tumor types, and predict disease progression with high accuracy. By integrating AI in digital pathology and radiology, healthcare institutions can streamline workflows, reduce diagnostic errors, and optimize resource utilization. AI-powered automation allows medical professionals to focus on complex cases while reducing workload. Despite the promising advancements in AI and digital oncology, several challenges remain: The integration of AI and digital oncology is revolutionizing cancer treatment, enhancing accuracy, efficiency, and patient outcomes. AI-based treatment algorithms, tele-oncology, and digital pathology are reshaping the oncology landscape, providing personalized, accessible, and efficient cancer care. As technology continues to evolve, the future of digital oncology holds immense potential in making cancer treatment more precise and patient-centric.AI-Based Treatment Algorithms & Risk Stratification
,Personalized Treatment Plans
,Risk Stratification
,Drug Discovery & Development
,Tele-Oncology for Remote Patient Monitoring
,Virtual Consultations & Follow-Ups
,Remote Symptom Monitoring
,Access to Specialized Care
,Digital Pathology & AI-Assisted Radiology Interpretation
,AI in Pathology
,AI in Radiology
,Automated Workflow & Efficiency
,Challenges & Future Prospects
,,
,Conclusion
,

Give us a call
+91 95605 38081Send Message
docvarungoel@gmail.comQuick Links
Services
Design & Developed By Tek Booster
(Digital Marketing Company)